Summary
Dr. Gustavo De Moraes discusses glaucoma imaging devices.
Question answered by:

Clinicians have a range of tools to help diagnose glaucoma and measure its progression. Imaging devices are an important part of the toolbox. You probably had an OCT (optical coherence tomography) test, which allows us to measure the thickness of the different layers of the retina and optic nerve. Just as a sonogram uses sound waves to create three-dimensional pictures of soft tissues inside your body, OCT uses specific wavelengths of light that are projected into the eye. When that light reaches the tissues, it flashes back how thick they are, producing three-dimensional and, cross-sectional images.
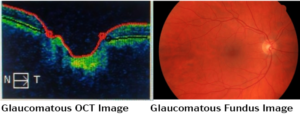
In addition to measuring thickness, in microns, the OCT technology also compares measurements of the patient being tested with a database of healthy people about the same age who don’t have glaucoma. (Green/healthy; Yellow/borderline; Red/ too thin/diseased.)
Sometimes, OCT images will indicate conditions other than glaucoma, such as a retina problem, and sometimes thinning over time may be the natural result of aging and not a reason to change treatment. Then the doctor has to rely on subjective experience and training and other tools – slit lamp exam of the optic nerve, visual fields, risk factors, and fundus photos, for example, to help interpret those findings.
In a small number of cases, the quality of the OCT may not be clear. For example, the machine will not be able to delineate those layers if the patient has significant cataracts or corneal haze.
Another long-standing imaging tool is a Fundus photo. The fundus is the inside surface of the back of the eye.
Fundus photos of the retina and optic nerve were used extensively before OCT was developed and are still used a lot today as part of a regular eye exam. Several optical coherence tomography (OCT) devices include color fundus photography capability. With a picture, you can always go back and make an evaluation – fundus photos can tell us more about glaucoma over time. Two photos taken at different time points can be compared side by side to assess progression.
Imaging aids the diagnosis and monitoring of glaucoma by providing objective documentation and measurements.
Recent advances in technology make OCT an indispensable tool in everyday practice. While the toolbox is growing, in the end they still require the doctor to interpret the results. But they already certainly help a lot. The future is with AI which will use those instruments to actually give us a ‘yes’ or ‘no’ diagnosis.
