Living With Glaucoma
One of the most popular features of TGF’s Eye to Eye newsletter and electronic newsletter has been our “Lifestyle Connection/Living with Glaucoma” series, in which glaucoma patients, inspiring and often courageous, have shared their personal stories.
People deal differently with the curveballs life tosses their way. That’s true in all facets of life, including how glaucoma patients cope with their diagnosis and with the reality of living with a chronic disease. We’ve asked individuals whose lives have been impacted by glaucoma to share some of their thoughts in the hope that their experiences can inform others.
Click here if you would like to share your glaucoma story or want to be added to our mailing list
Meet Nancy Tilson-Mallett, MD

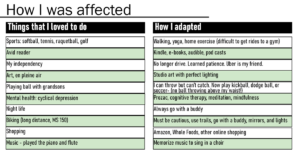
Adaptability has been one of life’s lessons for Dr. Nancy Tilson-Mallett. At the time of her diagnosis 23 years ago, she was a 46-year-old physician specializing in internal medicine, geriatrics, and hospice and palliative care, a mother, and an artist in Kansas City, Missouri.
“I was bumping into things; in my car, I had some side-swiping experiences while driving. The day I was diagnosed I learned that 80 percent of my optic nerves were gone. It was a depressing day in my life.”
Dr. Tilson-Mallett soon had a trabeculectomy in her left eye while taking a combination of eye drops in her right eye. A few years later she had a trab in the right eye as well. Her glaucoma has now been stable for several years.
“I knew I had lost a lot of vision and I was having a hard time navigating. But it took five years after my diagnosis before I knew I could do something about it. That was when I went to an occupational therapist who taught me all about dim vision and how to cope with it. It totally changed my life. Unfortunately, I hadn’t gotten that help earlier.
“There are things I can no longer do, but I have adapted. I loved sports but can’t see small balls to play with my three grandsons. So now we play soccer and frisbee.
“I was an avid reader. One of the reasons I retired as a physician at age 65 was that after 30 minutes of computer reading my vision would just grey out. And as physicians, we read all the time.
“Not driving was the most difficult thing. I can’t drive in the city as my peripheral vision is close to legal blindness.
“I think because I’m a visual artist, I use every nerve fiber I’ve got. I haven’t seen any studies asking if artists with visual impairments maintain better vision than other patients, but my theory is that they do.
“Once I learned that I had glaucoma, I really concentrated on color and objects, and memorizing what I see because I know I might lose it. I try to memorize my first impression so that’s what I remember without the dimness. And I’m teaching my husband the difference in colors such as ultramarine blue vs cerulean blue so that he can be more accurate in his descriptions to me.
“My passions for the love of nature, color and patterns, biology, and medicine are expressed in my artwork. Even in medical school, I saw the beauty in microscopic images. I’m fascinated with science and art and medical imagery.”
Dr. Tilson-Mallett still lectures here and there to medical students on keen observation and seeing. Her Vision Quest presentation depicts her glaucoma journey. “The technical images of my retina and optic nerve were fascinating to me,” she says. “The artwork is my interpretation of these diagnostic studies – mostly silk paintings.”
Her art is currently in a show titled “A Physician/Artist’s Visual Journey,” in partnership with Envision University in Wichita, Kansas.
As the gallery’s website states: “At the heart of this exhibition is her personal encounter with glaucoma. Fascinated by the technical images of her retina and optic nerve, she translates these diagnostic studies into a series of unique and visually stunning interpretations on canvas.”
“I also love doing landscape painting outdoors,” she says, “but I haven’t been able to do that since my mid-fifties because the lighting has to be absolutely perfect in terms of brightness. Instead, I’ve learned to do a quick sketch, do a color scheme, and take it back to my studio where there’s perfect lighting. I’ve learned how to pace myself.
“I am so grateful that my husband, who is passionate about historic preservation and has restored eight houses, is now transforming the old-fashioned attic of a 130-year-old house into my studio space, with windows on all sides”.
Meet Colleen Silveira

Colleen Silveira personifies the message that a glaucoma diagnosis doesn’t mean you should give up on what brings you joy and happiness. Look forward, not backwards, she says, and live your life to the fullest. She’s done just that!
A competitive athlete all her life, Colleen was diagnosed with Pigmentary Dispersion Glaucoma 12 years ago when she was 35. Early on, when she went monthly to get her pressures checked, doctors said her type of glaucoma seemed to be exertion-based.
“That really freaked me out! I didn’t want my life scaled back to just walking and yoga. I’m an endurance athlete! That’s part of my wellbeing for my mind and my body. Because I was training for Iron Man at that time, I asked my doctor if I could do a two-hour run and just run right in to the office for a pressure test. I thought that was the most accurate way to see if exertion was a factor in my eye pressure. We did this for about a year and found that my pressure never went up. That was a very interesting find for my doctors and a very happy moment for me.”
“Testing to get data is the only way to understand glaucoma better and seeing my doctor once every four months for pressure checks does not seem like good data. I was hoping something could be developed for us to use at home like diabetics had – to see what would, every day, affect our own pressures like food, time of day, lack of sleep or exercise. That was my number one concern – to understand what makes our own pressures go up or down.”
“I’ve been in the health care/wellness field and believe that food and nutrition can help change the trajectory of our lives. So, I started researching what foods could possibly help my eyesight. I would tell my doctor, I’m doing this, and trying this, and she would say, let’s see what happens. From drops and dietary ideas, I have been at a lower glaucoma pressure point in the last three years than earlier on my glaucoma journey.”
“One of my passions is international travel. I don’t do Iron Man anymore, but in my 30s I started to indulge in hiking. I wanted to see how other people lived and the way to meet indigenous people is hiking through their lands with them as guides. It’s beautiful and humbling. Now my husband is into that as well. It’s really a fun thing for us to do together – his first climb with me was Kilimanjaro!”
“I had never thought about altitude and IOP. Would my pressures go up climbing a 19,000 ft mountain? I asked my doctor, but again there was no data. Recently, when I was planning a September trip to Morocco to climb Mt. Toubkal in the Atlas Mountains, I was so thrilled that the home tonometer was now available and that I was able to get one. I took the tonometer with me to Morocco, tested every day, and found I was getting a little bit of an elevated pressure with elevation gains.”
“I just think it is so important when as glaucoma patients we can be in the driver’s seat in some of this. When we can take some power into our own wellness it gives us more of a sense of purpose in understanding this disease better.”
“I love going to unique places — 13 countries in Africa so far. Most recently my husband and I headed to Ethiopia, Rwanda, and Uganda. I was so thrilled to finally see these places, especially hiking to see the mountain gorillas! I went to the Ellen DeGeneres Conservatory where the good work of saving the gorillas will continue from Diane Fossey’s earlier work. Next year we’ll be going to Nepal. I’ll have my tonometer with me – 17,000 feet — and I will be able to test every night because we’ll be in a cabin setting and it’s just a gradual incline. It will be a perfect way to pressure test.”
“My passion for seeing the world is still there. I really hope that my eyes continue to do well so I can see everything. Every time I attend a conference about glaucoma, I see a huge change with new developments…we’re getting there. Have patience, keep informed, and enjoy your life in the meantime.”
Meet The Hill Family

“Our son, Jaxon, who was born prematurely, was three months old when we noticed that his eyes had a bluish grey tint and looked cloudy,” recalls Jasmyne Hill, who teaches at Houston Community College. “People kept telling us how big and beautiful his eyes were, but It was really his grandmother who told us that something just didn’t look right.”
Jasmyne and her husband Jermaine were referred to an ophthalmologist who immediately diagnosed the infant with primary congenital glaucoma. “As parents, we didn’t know anything about congenital glaucoma. When we think about glaucoma, we usually think about the elderly. We never knew a newborn baby could have glaucoma.”
Primary congenital glaucoma is a rare condition. According to the National Eye Institute, one in 10,000 people in the United States is born with the condition. It is bilateral (both eyes) and occurs more frequently in males.
“We had to do a lot of research ourselves just to understand what the doctor was telling us,” says Jasmyne. “We went on Facebook trying to find support groups.” “When we learned our newborn had glaucoma, it rattled us,” Jaxon’s Dad added. “There was a lot of stress; a lot of scary moments about my son being able to see.”
Jaxon has had three surgeries during his first year of life. “One week after the diagnosis, says Jasmyne, I had to hand my precious infant over to strangers in the OR at Texas Children’s Hospital for the first time. That was for a double goniotomy which was unsuccessful. Jaxon’s pressure remained high – in the 40s.
Three months later, the doctor put tube shunts in his eyes. After the surgery Jaxon needed four different eyedrops daily and ointment had to be rubbed around his eyes. The Hills talk about how difficult that was. Jaxon also had to wear eye pads so he wouldn’t touch or rub his eyes and his arms were padded too. “It was very hard for us to see our child suffering and not be able to help him at all.” Once the tubes opened up, which took time, he improved. A third surgery was performed to wash out blood in his eyes.

Jaxon is now 18 months old and is doing much better. “When we first started this process, we had to see the ophthalmologist once a week,” says Jasmyne. “As of now, we see the doctor once every two months. That’s a blessing!
“His pressures are stable and he is wearing glasses to correct an alignment problem and help him focus. Those are hard to keep on a busy toddler! While glaucoma is a part of his daily life, it doesn’t define who he is. Jaxon loves Cocomelon, playing hide and seek, annoying our pet cat, and playing with his trucks. He gets along well with other children at his preschool.
“We will not be able to know how well he can see until he can tell us verbally. We pray and try to stay positive! We are so grateful for Texas Children’s Hospital and modern medicine and technology that has come so far in saving vision for so many.”
What would the Hills want other parents to know? This is the first child for Jasmyne and for Jermaine, who came to Texas nine years ago from Georgia and works as a business analyst in the oil and gas industry.
“We feel other parents need to be aware that this can happen, and if you suspect something is wrong, find a doctor who will listen to you. Congenital glaucoma is often missed until after real damage occurs to vision. And because we now know that there is a genetic component to many glaucomas, including congenital glaucoma, it was suggested that we have DNA testing.”
Adds Jermaine: “This experience has motivated me to get regular eye exams myself –it had been years since my last exam. Everyone needs to be aware about glaucoma and know their family history.”
Meet Ericka

Glaucoma is not one single disease. There are different forms and types. Some are primary glaucomas and others are secondary glaucomas– meaning they are caused by another medical condition.
Ericka Shepard, a pharmacist and Glaucoma Patient Advocate from New Hampshire, has Iridocorneal Endothelial Syndrome (ICE syndrome) glaucoma, a rare and hard to diagnose secondary glaucoma which usually presents in only one eye. With this condition, cells on the back surface of the cornea spread over the eye’s drainage tissue and across the surface of the iris. This causes an increase in eye pressure, which can damage the optic nerve.
In 30 years of practice, Ericka’s glaucoma specialist at Tufts University in Boston had only diagnosed a few cases of ICE. The fact that Ericka did not present with distortion of the iris and pupil – a visible sign of the disease – made diagnosis still more difficult.
That was nine years ago, when she was 41 years old. Ericka had gone to her local eye doctor because she was losing vision. Sometimes for only minutes, but at other times for hours, a grey curtain would descend over vision in her left eye.
She was diagnosed with glaucoma and sent to a glaucoma specialist at Tufts University who over a period of months prescribed numerous different eyedrops. But they did not lower her IOP. When she was finally diagnosed with ICE (a diagnosis that can be aided with spectral microscopy, which visualizes changes in corneal endothelium cells), an Ahmed Shunt was surgically inserted to aid drainage. The cause of ICE syndrome is not known – some think that it is virus-related. What is known is that it normally affects only one eye, often in middle-aged women, and that it appears not to be hereditary.
“My advice to all,” says Ericka, “is if you are a middle-aged woman experiencing vision problems in just one eye, have unilateral glaucoma, and no family history of glaucoma, you should ask your doctor about testing for ICE using specular microscopy.”
Ericka did well for several years, but last July her pressure rose again. “We knew the shunt was probably blocked,” she says.
“My pressure was in the 20s in the office, which was not unusually high for me, so we assumed we had some time to determine the next step. Since there aren’t many studies with ICE patients, my doctor and I decided to get multiple opinions from various specialists…one of them suggested I rent a home tonometer. The tonometer rental showed that my IOP was spiking into the 40s in the morning and sometimes in the evening. We knew we had to do something quickly with so much fluctuation and so I had a Baerveldt shunt implanted into my eye. It’s brought my pressures way down!” While I know that at some point this will probably fail due to blockage, hopefully by then something new will be available.”
Ericka’s experience with a home tonometer led to her becoming a Glaucoma Patient Ambassador. Trained as a pharmacist, she has 25 years of experience working at CVS. At one point she was District Manager for 15 stores, but she left that job when she became pregnant with twins. Today she works as a pharmacist one day a week.
As a home tonometer user, in December 2022 she received a general email from MyEYES, who were reaching out to all their patients looking for Ambassadors to provide support to new home tonometer users.
“When they receive a physician’s prescription for a home tonometer, we call the new patient immediately and stay with them all the way through their home tonometry journey. Doctors’ offices are busy, it is critical to know your disease, be compliant with your current plan, and follow diagnostic measures like renting a tonometer to improve outcomes.”
“It’s been amazing talking to hundreds of patients, all with different stories. It’s very gratifying to know that I can share my own experience and be part of their glaucoma journey.”
Meet Pat

Abstract Artist Pat Caulfield of York, Pennsylvania was diagnosed with glaucoma 11 years ago. As a glaucoma patient with vision loss, she believes it’s crucial to be your own best advocate. “It’s one of the most important things I stress when I give talks. There’s so much good information out there,” she says, “and there is no reason not to know more about this disease. If you don’t do the research, you won’t know what questions to ask.”
As a professional artist, Pat has been working hard to create awareness and education about the disease through art. “I believe that the practice of art can heal and can help, and can help express yourself in different ways through art and creativity even if you don’t have 100 percent of your vision.”
With three shows of her art this past year, her work as a resident artist at a local gallery and through her social media presence, Pat has long used art to reach out and educate. Just now she’s working on a proposal for a gallery to mount an interactive display of works by visually impaired artists. Her unique idea is to give gallery visitors blindfolds with holes in each of them and ask them to look at the art and then draw what they see on a wall. The point she’s making is that vision loss doesn’t follow a pattern – every person loses vision in an undetermined way. Glaucoma isn’t a cookie cutter disease. It affects each person’s diagnosis and vision loss differently and different methods of treatment must be utilized to encourage the best outcome.”
Pat’s glaucoma was first diagnosed during a regular eye exam when she was 55. “I was shocked,” she says, “and went to see a doctor who immediately prescribed laser surgery. I said, ‘no,’ I need to learn more first. And then I went to the Wilmer Eye Institute at Johns Hopkins Hospital in Baltimore, where my doctor confirmed that I had glaucoma but didn’t think laser would help. After five successful years on eye drops, my specific drop was discontinued and none of the many drops I tried seemed to work. Then, all of a sudden, I lost almost half my vision. With pressures up to 46, I immediately had surgery for a Baerveldt Shunt on my left eye. That worked for a while. But then I started losing central vision in the right eye. My rapid progression, not the norm, just ripped through. I then had trabeculectomies done in both eyes. It was terrifying!
“I had been a successful kitchen/bath designer for over 20 years. But about the time I lost my central vision I had to make some changes. I don’t drive as much anymore – locally but not on the highway. I stepped back from my design career and started taking my art more seriously. I took courses, then taught art history at a local school. I’m very active in our regional art world and beyond.” Pat has successfully curated two art shows for visionally impaired artists on the West Coast. She has also just been selected as one of three women artists for an upcoming show in Lancaster, PA.
For the past two years Pat has been a guest lecturer, speaking to honor students in the neuroscience department at Boston University about vision loss and the internal process of creating art. “We talk a lot about the way it affects how you create – both intellectually and emotionally. We discuss how colors are affected with cataracts and that details can become lost with the progression of glaucoma.
“Through my outreach, I have met incredible people with such tenacity and strength,” Pat says. “One woman is a medical doctor in India who is now legally blind from glaucoma. She’s creating an outreach program in India for people with glaucoma to come in and enjoy expressing themselves despite their visual impairment. Then there’s a gentleman in London, with only five percent of his vision, who uses braille as full-scale interactive art and teaches blind children how to read his paintings. I never would have met these people if I didn’t have glaucoma myself.
“While I’ve already lost a lot of vision, a few weeks ago my doctor confirmed that my vision was stable. I just hope I can maintain the vision I have now for the rest of my life. I’d be perfectly content with that!

Patricia works in mixed media on birch cradleboard and paper using acrylic paint, collage, oil pastel, oil sticks, pencil, watercolor crayon and vine charcoal along with sanding and distressing.
Meet Amy

Amy Dixon is a visually impaired professional triathlete (swimming, cycling and running). Among her lengthy list of accolades, she’s a 4-time cycling and triathlon national champion, and was a member of the Tokyo 2020 US Paralympic Team.
Amy began losing her eyesight in college some 25 years ago to a rare form of uveitis, an autoimmune disease, which led to devastating forms of glaucoma. She has two percent of her eyesight remaining in one eye only.
As if her athletic accomplishments were not enough, in recent years Amy has taken on another vocation with passion – as a patient advocate. During the year the Paralympic Games were delayed due to Covid, Amy was extremely ill. Her autoimmune disease came out of remission once again, leading to surgery which ultimately led to embolisms in both lungs.
Amy is President of Glaucoma Eyes International, which includes the online support group Glaucoma Eyes. “Giving back to those who have helped me through 39 surgeries in the last 10 years and to the visually impaired community is hugely important to me,” she says.
“We serve about 30,000 patients worldwide, not only through the support group. We have a team that addresses individual requests – helping patients gain access to physicians, lower cost surgeries and free or lower cost medications from our pharmaceutical partners.”

She is also the founder of Camp No Sights No Limits in San Diego, her home base. “It’s the first-ever camp dedicated to producing elite-level blind triathletes,” she explains. “In my training journey, I discovered there was no coaching that was specific to blind athletes who are capable of world class competition but needed guides, tandem bikes, skills and resources to get to the top. I wanted to reduce these barriers and educate new athletes. We’ve had 46 graduates – two campers actually went on to go to the Paralympic Games in Tokyo – a huge accomplishment! Camps are planned for San Diego and in Tennessee this year, along with local clinics throughout the country.

“One of the things I’ve found is that there is a great communications gap between the patient and the doctors. They might give you general contact info for low vision resources, but there are better resources out there with all the new adaptive technology that can help people to continue working and being contributing members of society. I got frustrated that people didn’t know about the different phone apps for blind or visually impaired users and other more costly high-tech aids. So, I talk to doctors and their staff about having these conversations with their patients. I want to make all that more accessible BEFORE people become low vision and need it desperately.
“I work with different medical tech and biotech companies advocating for coverage by Medicare and other insurance companies so these advances become more affordable for people with low vision. I also work with the sales force at various pharmaceutical companies, like Allergan and Bausch and Lomb, to teach them how their products are changing lives, to humanize their experiences. I have the pleasure to work with corporations to maximize disability inclusion and mental health support in the workplace.
“My goal is to make sure that when patients leave their doctor’s office, they feel empowered; understanding the seriousness of their disease but having all the tools and resources on hand to continue working to manage their disease financially and medically. I want people to feel seen, heard and important.”
Meet Susan

When we first met Susan Genis in 2009, she had just been diagnosed as “legally blind.” “I probably could have been diagnosed years earlier based on my reduced visual field from advance glaucoma,” she says; “but that legal determination was an awakening, allowing me to receive all sorts of mobility-oriented help and various devices to make my life easier. I’ve been dealing with vision issues for some 50 years. It all started in my 20s, after years of extreme myopia – first uveitis, then cataracts and glaucoma.“
Recently, we met Susan again. An active 74-year-old New Yorker, she has lost all vision in her left eye and undergone several surgeries in the right — a stent implant and a partial cornea replacement.
Susan is a former criminal lawyer and yoga instructor, who still teaches yoga to seniors on Zoom. “Since we first met, I have discovered so many activities in the city for people with low vision that I never knew existed. So, in spite of it all, I’m busier and I’m happier.”
She points out that most of the art museums in the city offer a range of free programs for people with low vision – among them MOMA, the Met, the Whitney and Guggenheim museums. “That’s been fantastic.”
“Then I discovered a non-profit organization that does tandem biking for people with disabilities. You just sign up and they match you with a volunteer ‘captain.’ It’s usually a two-hour ride, these days in Central Park – but only when it’ s over 40 degrees and dry. What a feeling of freedom!”
Susan has done the five-borough bike ride. While currently not riding because she’s on the mend from a fractured pelvis, her goal is to do the five-borough ride again next May.
“The captain in front does the steering and changes the gears and handles the brakes. The captain serves as our eyes and controls the ride. But we both pedal so you have to be in synch. The essence of tandem biking is communications. I like going fast. It’s a nice workout”.
For the last four years Susan has been a member of the chorus at the FMDG Music School, which is specifically for people with visual impairments. “They accommodate with large print music, braille music, and audio cassettes. “We recently performed at the Met Museum’s Cloisters, and there’s a law firm that supported a performance in their office building’s lobby. In the spring, the chorus is scheduled to perform at the Met Museum – a combined project of music and art.”
She’s also a longtime steering committee member of the Glaucoma Support and Education Group, which meets monthly, now on Zoom, for a Saturday lecture by leading glaucoma experts to learn about and discuss innovative new approaches to glaucoma diagnosis and how to manage the disease.
“I don’t think I could live outside New York because I know the city, and there are so many options here – buses, subways, taxis. Mostly, public transportation has served me just fine. But since my accident, I haven’t really taken the subway, even though I find in some ways it is easier because I know the stops. At the moment, I’m using the Access- a-Ride service and taxis more. I love that a lot of the newer buses announce the stops and I find that most people are really helpful when I need assistance.
I’ve lived in my apartment for over 40 years so I know it and I know where things are. As I cannot read print of any kind, I rely completely on magnifying glasses and have several devices. I have a large screen computer and I have everything magnified. And when I use my iPhone, I dictate into it. I have the Be My Eyes app, and while I don’t yet rely on those things, sometimes I’ll ask – ‘what does this say,’ or, ‘what street is this.’ I have different canes – they give me a sense of where I’m at.
“Considering it all, I’m doing really well,” Susan says.
Here are the websites for some of the activities Susan has suggested in New York.
FMDG Music School—for children and adults with visual impairments https://fmdgmusicschool.org
InTandem Cycling—for anyone who is unable to ride a bike alone https://www.intandembike.org
NY Public Library Services for Blind and visually impaired https://nlsbard.loc.gov/login//NLS
Andrew Heiskill Library Braille and Talking Book Library https://www.nypl.org/locations/heiskell
Glaucoma Support and Education Group
Email: gseg@glaucomasupport.org
Meet Hillary

Until two years ago, Hillary Golden, a Louisianan living in Denver, didn’t know a lot about eyes, and even less about glaucoma. But what a difference two years can make! Today, as a 53-year-old with severe glaucoma, her life is steeped in learning as much as she can and spreading the word about glaucoma, specifically about normal-tension glaucoma (NTG).
“I have been in medical sales my entire career,” Hillary explains – “from selling CT scan equipment to medical software.” She was training oral surgeons on computer-guided surgery in 2020 when elective surgeries were halted due to the Covid pandemic. She was furloughed for four months. It was during that period at home that she noticed a stye on her eyelid and decided to get it checked out.
“I had the time, so I agreed to do a more comprehensive eye exam. The assistant dilated my eyes. Then the doctor came in and looked in my eye and says ‘hmmm, I don’t like the look of your nerve.’ At this point, I knew nothing about eyes. They seemed more concerned about the nerve than about my stye. I remember that at about 11:45 she said: ‘I think you might have glaucoma.’
“I came back for a visual field test and OCT imaging test which confirmed that I had severe glaucoma – they said it was normal-tension glaucoma. A few days later I saw a glaucoma specialist who started me on eye drops. That was the beginning of a whole learning process. I wanted to research the heck out of it – what is normal tension, what does it mean? I thought only old people got glaucoma!”
Normal-tension glaucoma is a form of glaucoma in which the optic nerve is damaged even when the pressure does not exceed the normal range. “Because I was miserable on the drops, they said we could try SLT laser surgery, but that did not work. I had lost 40 percent of my visual field in both eyes at my diagnosis. The loss is in the upper nasal quadrant, so thankfully, I can still see and can drive.
“In 2021 I was traveling again, working for Allergan, selling a medical device for glaucoma. I got more involved with my eyes – I was talking to glaucoma doctors all day for work. This past February I changed jobs moving to Sight Sciences –working with the Omni MIGS surgical system for glaucoma. The reason I love my job is because I want to help other people through the doctors I call on every day. I also want people to know that normal-tension glaucoma (NTG) is different.
I personally mentor a couple of glaucoma patients and I am in several glaucoma support groups where I answer questions the best I can and give support to whoever needs it. In the U.S. normal-tension glaucoma accounts for about 30 percent of all glaucoma cases.
“I’ve done a lot of research on my own. There’s a prominent doctor in Switzerland who has done research on the role of vascular dysregulation in NTG and he’s been helping me. I also have a doctor in Denver and one in South Dakota. I’ve tried to seek out the gurus of normal tension…I have to try everything.
“I have a home tonometer – I think this is going to be the norm – measuring IOP three or four times a year in the doctor’s office just isn’t often enough. It’s super important for my pressures to be super low – they need to be 9 or 10. I have a tech background. But not everyone is tech savvy – more doctors need to have a technician to help patients set up their tonometers.
“I’ve also become a certified health coach. I know it’s going to help that I eat well and take care of myself in other ways, but it’s frustrating. I’ve lost so much vision and I sit in the waiting room with all these other patients who are 20 years older than me, and my eyes are worse than theirs. It’s stressful thinking about what my eyes will look like in 20 years. Losing vision is a scary thing — I’m doing everything I can to preserve what I have left.”
Meet Greg
After 26 challenging years, most recently losing all his vision in one eye, Greg Alter believes that people who live with glaucoma shouldn’t give up. He has hope, he says, that one day soon lost vision can be restored and people with glaucoma will get their vision back.
With the loving support of his family, and the ongoing advocacy and activism of his mother, Lela, Greg has courageously faced the issues of his life. He was born prematurely at 23 weeks, weighing only one pound. After spending 10 months in intensive care, and another four months in a rehab unit, he came home for the first time at 14 months. In an article he wrote while in high school, Greg thanks the doctors who saved his life and the therapists who helped him learn how to talk, walk, and use his hands. Because prematurity can also cause vision problems, he had a laser procedure as an infant and eye examinations annually.
One of the issues his parents advocated for was regular education. “We always wanted Greg to be mainstreamed,” Lela says. Greg agreed. He did well, finishing high school in New Jersey with good grades and a regular diploma. “We were planning for college,” says Lela Alter.
“But we weren’t aware that Greg had a spinal issue, a result of his prematurity,” she explains. When he returned from a trip to Israel in the summer of 2017 – a lifelong dream – the pain was excruciating. That led to paraplegia, and very difficult spinal surgery to avoid total paralysis.”
In 2019 Greg started to complain about flashes in his right eye,” Lela recalls. “We took him to three specialists who changed his eyeglass prescription, but there was no mention of glaucoma or the need to see a glaucoma specialist. Then Covid struck.
In June of 2021, Lela noticed that the right lens of Greg’s eyeglasses was slightly cracked, which, to her dismay, Greg hadn’t noticed. After just a few minutes at the ophthalmologist, the doctor said, “Your son does not have vision in his right eye.” Greg was diagnosed with closed-angle glaucoma.
“At that time, we knew nothing about glaucoma and I assumed his vision would return when his pressures lowered. Since then, Greg has seen ‘tons’ of glaucoma specialists– I’ve reached out to doctors all over the United States looking for hope.
We have had to change college plans. Greg took a class at Bergen Community College this summer – but it’s very difficult for him with his eyes right now given all the reading he has had to do. It has been daunting.”
For Lela’s part, she has become an ardent advocate for glaucoma awareness and intensified research so that vision restoration can be achieved. She prays it will happen during her son’s life span. She wants to make sure that children are tested for glaucoma at the earliest age possible – too many people still believe glaucoma is a disease of the elderly, she says. She asks others to speak up, to support research, and to urge research centers around the world to work together. “I have to believe that vision restoration can be accomplished,” she says. She looks to other diseases as examples of what advocacy and activism can achieve.
Meet Bernard

I really think that testing for glaucoma should be mandatory. That would help! Glaucoma may not be curable, but it is manageable and the earlier you know it, the better!
Hello, my name is Bernard. I am 65 years old, retired and I live on the twin island paradise called Antigua and Barbuda, in the heart of the Caribbean. It lies about 300 miles East of Puerto Rico.
My personal relationship with glaucoma started when I was about 30 years old. My father was diagnosed with glaucoma several years earlier, but then, I only knew that a) it is an incurable disease of the eye, b) it is not contagious and c) left unchecked, it progressively, painlessly (in most cases) and almost imperceptibly, robs one of sight – permanently!
I am astigmatic, or near-sighted. My parents realized that I was having difficulty in school, so a visit to the doctor, then to the ophthalmologist, and glasses were prescribed. I wore prescription glasses since I was 7 years old, but there was never any discussion about even the possibility that I may develop glaucoma. Several visits to the ophthalmologist over the following years checked my vision and adjusted my prescription strength. Back then, testing for glaucoma was not considered as a first step.
Dad eventually went blind due to cataract surgery that didn’t work out. Then, cataract surgery was major and there was a very stringent regimen of dos and don’ts, which he didn’t always follow!
As I grew older, it dawned on me that somewhere along the path of life, I could develop glaucoma, and/or be sight challenged. One year whilst on vacation in Miami, an eyeglasses franchise was advertising 2 pairs of glasses for the price of 1. To cash in on this deal, one had to have an eye exam. It sounded like a great idea to me. At the time, my lenses could not have been prepared in Antigua and so the doctor would have to send the prescription to the US to have the lenses made and then shipped back to Antigua, which worked out very expensive and of course, a long wait time to receive the glasses. So, it was worth finding out if this could be done quicker and cheaper, in Miami.
What started out as a normal and routine eye exam, quickly escalated to a near full-scale emergency. The doctor was in a state, to put it mildly! Several hushed conversations, urgent phone calls, more conversations…finally, he came to me to say that he had managed to secure a place for me to have laser surgery…the following morning! Well, okay…my turn to be in a state now. SAY WHAT! He explained that my intraocular pressure (IOP) was very high, which in turn had damaged my optic nerve.
Glaucoma???
Yes, glaucoma! So, the surgery would be necessary to relieve the pressure in the eye on the optic nerve…
I have glaucoma! I have glaucoma, like Dad, I have glaucoma…
‘Did you hear what I said?’ the doctor said…
’Huh, What, I, I didn’t hear you’…
…thinking again…I have glaucoma!
To cut a long story short, I arranged to stay on, had the laser surgery and the aftercare, then returned home with my now confirmed new partner for life – Glaucoma!
Why was this such a shocking revelation to me? Why was I not tested before? I would have had glaucoma for several years by that time and I was totally unaware! At age 30, one feels invincible, or that ‘this could never happen to me!’ But this is glaucoma, in general, no pain or discomfort, no noticeable defects, unless you have the proper equipment. It puts a whole new meaning on ‘look deeply into my eyes!’ But in the early days in the Caribbean, the equipment wasn’t available and where it was available, the costs were prohibitive!
My 2 boys are now adult men. The eldest shows no signs of glaucoma while the second has been on eyedrops for a few years now. He has not lost any vision at this time, nor does he need to…provided that he administers his drops daily and consults his doctor regularly re: the management of the disease. For me, this is the worrying part. Remember my comment about being 30 and invincible? Hence, this has become a regular part of our conversations; ‘Did you use your eyedrops?’ or ‘don’t forget to put in your drops!’
Glaucoma is not something you see, feel or notice, nor is it something that someone can see by looking at or speaking with you; ironically, it simply prevents you from seeing, slowly (so you hardly notice that you are losing sight) from the periphery of your vision closing into the center, usually painlessly, progressively– permanently! Get tested today! You won’t regret it.
For your children, you want the best for them, to see them excel and ensure that they have all the skills and tools that they need to sharpen their ability to succeed in today’s very competitive environment. Get them tested for glaucoma. Neither you, nor they, will regret it!
Get Tested!
Get tested early!
Get tested as part of your routine annual checkup!
Get tested – PLEASE!
I will end with the words on one of Antigua’s Glaucoma Week banners: –
DON’T LET THE SUN GO DOWN ON YOUR SIGHT
Meet Joe

Joe Rosen, one of TGF’s newest board members, has had a long and successful career in the healthcare field. Trained as a CPA, he started a business that collected human blood plasma for further manufacturing into albumin, gamma globulin, antihemophilic factor, and other products with medical uses. Joe focused on the business side of the company, which grew to become the largest independent collector in the industry – at one point with collection sites in 26 states.
Yet he admits he knew very little about glaucoma until it impacted his life personally. That was over 10 years ago when his wife was diagnosed. Today, while he still works part-time, Joe is a caregiver and major support for his wife and is a supporter of glaucoma research initiatives.
It was during a routine eye examination at a local ophthalmologist in New Jersey that Mrs. Rosen learned she had the first signs of glaucoma and should see a specialist. “When you first hear the word ‘glaucoma’, and you know nothing about it other than you could go blind, it’s a shock!” Joe recalls. “It was distressing to both of us.
“We went to see Dr. Robert Ritch and there was an immediate level of comfort. Whether we believed it or not, he said ‘you will not go blind – I will take care of you.’ Our anxiety level went down – he was someone we trusted.”
Over the years, Mrs. Rosen has had laser treatment, surgery, and she is dutiful about her eye drops. “I’ve heard that compliance with taking medications is an ongoing challenge for the profession, but my wife is the most methodical and diligent patient in terms of how she instills her eye drops,” Joe explains. “She’s watched ‘how-to’ videos and in all these years, I can’t remember her ever missing one of her drops – even when we were traveling worldwide. If you asked her about that, her response would be: ‘What do you expect – these are my eyes. I will do whatever I can to follow exactly what the doctor says.’
“When it comes to taking visual field tests, she hates them. The anxiety is immense, as is waiting for the doctor to say ‘there hasn’t been any change.’ I imagine most patients would feel the same way. She participated in several of Dr. Ritch’s research trials, including one that concerned an alternative to the visual field test.
“Since joining the TGF Board I have become more involved as I want to understand what someone with glaucoma goes through. I listen to the Webinars we present. I think they are very good. Even if you don’t grasp all the science being presented, you learn what’s going on – new treatments, research, diagnostics. Education is a great benefit to patients – I think that’s so important.”
“I continue to try to be as supportive and understanding as I can be.”
Joe has been on the Boards of several not-for-profit organizations as well as Boards of private and public companies in the healthcare sector. “I was happy to join the Board of the Glaucoma Foundation, an organization that was financially sound and structured for the benefit of the glaucoma patients it serves.”
Meet Kumar

Kumar Mahadeva, a TGF Board Member since 2014, was born and raised in Sri Lanka. Following the example of his parents, he went to England to attend college. He had intended to return to Sri Lanka after college. But because the country was at the cusp of a civil war, he instead came to the U.S. to attend Harvard Business School. “I had always hoped to return to Sri Lanka, but I’m glad that I stayed in the U.S.,” he says.
Indeed. As the founder of Cognizant Technology Solutions (CTSH) in 1993, and its first Chairman and CEO, Kumar was the driving force behind one of the fastest-growing technology services companies in the world. Cognizant has grown into a leader in its industry and is in the S&P 500 and Nasdaq 100.
“Cognizant leveraged talent in India to deliver large software projects to clients worldwide, a pioneering concept at the time. Although remote work has now become routine, the infrastructure for it did not exist back in 1993. The internet was not what it is today, and we had to build our own networks, Software platforms and videoconferencing systems to integrate widely dispersed teams. In the end, we got the model working very well. There is a tremendous shortage of talent in technology, and the U.S. benefits from having access to a global talent pool.
“I got involved with The Glaucoma Foundation because I was a glaucoma patient myself. I was diagnosed around 2003 but was not prescribed any treatment. Fortunately, I sought a second opinion from my current doctor, who said my pressures were far too high. And so, I learned about the risks of glaucoma creeping up on you when you don’t even realize it, and also how different it can be depending on how you are treated and cared for.
“I do drops and had one surgery – other than that, things have gone well. Up to this point, glaucoma hasn’t changed my day-to-day life.
“Given my personal interest in glaucoma, I looked up organizations I could contribute to and became a regular contributor to the Foundation. Then they reached out and asked me if I wanted to join the Board.
“For me, the Foundation is both an opportunity to contribute to something that is meaningful to me and also a tremendous learning opportunity. I am particularly interested in some of the more fundamental aspects of glaucoma research into the causes of glaucoma that can eventually lead to a full cure rather than just management of the disease.
“So, more recently, when the Foundation was looking for funding for several research projects, I agreed to support a very fundamental piece of work on blood flow to the eyes and the neurons and pericytes which control that blood flow but which in glaucoma patients are not working so well. Now the research team on this project at the University of Montreal has unveiled mechanisms underlying these defects. Their findings have just been published in the Proceedings of the National Academy of Sciences USA.
READ THEIR PAPER HERE
“My interest in finding a cure is heightened as glaucoma is hereditary and such research might benefit my young son and others of his generation.
“I’m active in several other organizations whose work interests me personally, such as the Cure Alzheimer’s Fund, where I recently joined the board of trustees. My father had Alzheimer’s disease, which prompted my interest in the disease.
“What do I do for fun? My 20-month-old son is certainly entertaining. I’ve always been a technology nerd, so I do a lot of things in that area. We also enjoy a culturally full life in New York and Miami Beach.”
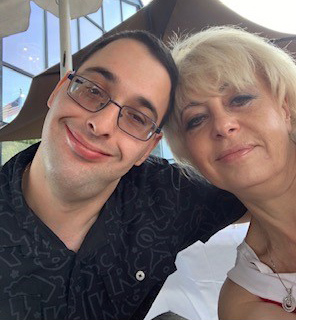
Meet Jahkori

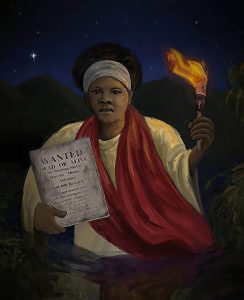
Jahkori Dopwell Hall is an inspiring 21-year-old artist, currently a senior at the Ringling College of Art and Design in Florida, where he’s majoring in illustration and minoring in art education. His painting “Mrs. Black Moses, a portrait of the American abolitionist Harriet Tubman, won the TGF Art Challenge Award for Favorite Artwork based on audience voting of this year’s Art Challenge submissions. The honor carries with it a prize of $500.
Jahkori is passionate about his work, overcoming significant challenges. He was born with primary congenital glaucoma, a rare condition that affects one in 10,000 infants. Some readers may be familiar with Jahkori’s story which he shared as a panelist on a TGF webinar earlier this year. In it, he addressed the importance of trust between physicians and glaucoma patients. He credits his doctor of 20 years who, with his team, has been with him every step of the way.
“My ideas come from a combination of my imagination and things experienced in life,” says Jahkori. “My goal is to make a statement with my art and bring about change in the community.”
Glaucoma has affected Jahkori’s life physically, personally, and professionally, he says. “Eye surgeries, visual fields, OCT imaging tests, eye patches – it was all too much for a growing child like me. But I always had a passion for drawing and painting and was not aware that my glaucoma could put that in jeopardy. Since I had my first goniotomy surgery, my right eye has been stable and that eye maintains 20/20 vision to this day. But my left eye continues to fluctuate with high pressures and blurred vision.
“I’m living proof you can achieve whatever you set your mind to,” says Jahkori. “When I took my career path to a new level, people told me I wouldn’t be able to do that – but I didn’t let that negativity get in my way.”Jahkori has had his art displayed in many places, including Lincoln Center in New York, and he’s received several commissions including a contract to design and paint an abstract mural for a financial services building in Sarasota. He also teaches art to children as a substitute teacher and privately on weekends.
“At the end of the day, people are going to tell you who you are. But you have to punch back and say ‘no’, this is who I am. I was able to see the path, even with blurred vision.”
Meet Terri

The Ophthalmology Specialists’ Secondary
Waiting Room by Terri Kirby Erickson
Light is gentle here, and scarce—a room designed for dilated pupils, for patients with glaucoma, cataracts, and macular degeneration—people whose eyes have somehow failed them. Several wear dark sunglasses. Others blink and blot their eyes with tissues. At various times, every chair is taken. Then, a name is called, and after that, another. But no seat is vacant for long. There are so many of us, and so few hours left in the day. While we wait, some engage in whispered conversations. We compare eye pressures, past surgeries, and treatments, share stories like cowboys gathered around a circle of slowly-dying embers—though most people sit in stoic silence, watching the wall-mounted TV, checking their cell phones, or staring into space. One elderly woman leans over her walker and shouts, She, pointing to her middle-aged daughter, keeps shushing me. And when her daughter says, with harried affection, Shhh, most can’t help but smile, faces illuminated like priceless paintings by the faintest, yet unbearably beautiful, light.
Award-winning poet Terri Kirby Erickson, a North Carolinian, launched her sixth published collection of poetry, winner of an International Book Award in Poetry, in late 2020. She also has the unique distinction that her “Poem by a Woman with Glaucoma”
was just published in the Journal of the American Medical Association (JAMA) in their Poetry and Medicine section. Terri has always actively marketed her work and TGF learned about her when she contacted several ophthalmologists and organizations like TGF about the poem. “As a poet,” she says, “you just want to have your work read and hope that people will be moved by something that you write.”
Terri doesn’t just have glaucoma – she’s had her fair share of medical issues and thinks it’s important for medical journals to get some perspective from patients and not just healthcare workers.
“It’s so necessary that people feel they are not alone with their afflictions. A poem can go straight to a person’s heart in a way no other kind of writing can do,” she has said. “Poems unite and connect us to one another’s humanity. Every poem is another little light in the darkness, telling us that we are not alone.”
Although Terri’s been writing since the 5th grade and worked in the fields of editing and writing for years, it was when her daughter left home, “a strange time for a parent,” that she started to think about what her new passion might be. Attending a performance at Salem College by former US Poet Laureate Rita Dove, she says she knew “this is it – it’s what I want to do.”
“That’s when I got started. I just started writing and writing and actually self-published my first book. I was teaching a course at Salem College for adult students in poetry and ended up doing an interview on the local NPR station that came to the attention of Press 53 – the press that has published five of my collections.”
“I just love her way of describing things,” said Kevin Morgan Watson, publisher and editor in chief of Press 53. “When you’re reading her poems, you feel like you’re there. You can taste the air. You can smell the flowers. You can hear the birds flying overhead. It really is amazing. She is the queen of metaphor and simile.”
Terri also has Crohn’s disease and her first diagnosed eye disease was Fuchs endothelial corneal dystrophy, which affects the thin layer of cells that line the back part of the cornea. “My corneas are like lace doilies and can tear easily.”
“I’ve had several laser surgeries for my open angle glaucoma and have spent a lot of time in doctors’ waiting rooms. But I’m lucky that everything was caught early. As a writer and someone who is very visual, the idea of having a disease that could lead to partial or full blindness was truly scary.
I just feel extremely grateful and happy that I was able to find success doing the thing i I decided that I really wanted to do, and that I had a passion to do. I plan to live my life to the fullest – hopefully for a long time.”
Meet Barry
By anyone’s estimation, Barry Friedberg is living a very full and active life. An investment banker and philanthropist, Friedberg has been a glaucoma patient for over 30 years. He’s had laser and cataract surgery, two trabeculectomies and shunt procedures in his left eye, one trabeculectomy in his right eye, as well as a corneal transplant and macular pucker and macular edema in the left. Acuity is 20/200 in his left eye and 20/40 in the right. Neither is correctable.
“I get great treatment, he says. I’ve got doctors for these various conditions and I see them all regularly. I’m very fortunate. I haven’t given up anything except that I no longer drive a car. My goal is to just keep doing normally as much as I can.”
Barry Friedberg puts in a long day as co-chairman of the board of New York Private Bank and Trust – these days working remotely on the phone and via Zoom. He also remains very active with the New York City Ballet, where he was chairman of the board; is a trustee of SCAN-Harbor, a group that works with inner-city kids in East Harlem; and serves on the board of The Glaucoma Foundation. Earlier this year Friedberg and his wife Charlotte Moss established the Foundation’s first named research grant.
Anything you do that is good for your cardio/vascular system is likely to be helpful, he advocates. For his part, he exercises most days and continues to play golf and to ski.
What advice does Friedberg have for newly-diagnosed glaucoma patients?
“A heart healthy diet and regular exercise. Most important – you must listen to your doctor and be incredibly disciplined about your drops,” he says. “I’ve thought about why compliance is such an issue for glaucoma”, he adds. “I think part of the problem is that usually, when you take medicine, you expect to get better. With glaucoma, it’s different. You must take your medicine to keep your glaucoma from getting worse. Without taking your drops, you may not notice any slow changes, but they are taking place!”
“It takes motivation. My motivation is to enjoy an active life with my family and friends and be a contributing partner in my business and philanthropic activities.”
Meet Christine

In 2017, Christine DiSomma was diagnosed with glaucoma.
This is her story.
I had never been to an optometrist/ophthalmologist before. What drew me to go see the doctor was trouble reading, and I was experiencing red eyes. Honestly, I just thought I needed reading glasses.
When the doctor did my eye exam, he noticed I had a hemorrhage in the back of my left eye. He then performed an OCT scan and that is when he told me that I had severe optic nerve damage. Then he said,
“You will go blind.”
He was awful. He said that to me point-blank, with no remorse. Earlier that year, I had a hysterectomy due to cancer, something that he was aware of. He then proceeded to tell me I was having a “real bad year.” I remember leaving his office scared and upset, crying the entire way home.
My father has glaucoma, so I knew a little bit about the disease, but I was never that concerned about having it. It was never something that was discussed.
My husband’s friend Dr. Brian Rosenblatt is an optometrist, so we went to see him the next day for a second opinion. He was wonderful. He spent a good 2 hours with us explaining everything he had discovered and the next steps I needed to take.
I left him feeling a bit more optimistic.
Dr. Rosenblatt recommended that I see Dr. Robert Ritch for treatment. I see him every 3 months. We found a combination of eye drops that work for my pressures. I also take oral supplements that Dr. Ritch has recommended. I had SLT surgery in both eyes.
In the beginning, there was an adjustment period, but it has now become my routine.
I am not going to lie, when I first met Dr, Ritch, I was a bit intimidated. I realized shortly after, he wants the absolute best for his patients and does not accept anything less than 110% from anyone who works with him, and I respect that. It is something you want to see as a patient.
Dr. Ritch has taught me so much.
He taught me that I can control this disease.
He has never once made me feel that I would spend a day alive without seeing.
My advice is, go to the eye doctor regularly. Do not wait until you think something is wrong.
If I had started earlier in my life, I would have been diagnosed sooner, and would not have lost so much of my vision. Listen to your body and what you think is right.
Robert Ritch, MD is the founder and medical director of The Glaucoma Foundation. He is the Shelley and Steven Einhorn Distinguished Professor of Ophthalmology, Chief of Glaucoma Service, and Surgeon Director at The New York Eye & Ear Infirmary.
Meet Lilian

In her professional life, Lilian Rosenbaum, LCSW-C, BCB, PhD, has been an acclaimed pioneer in the field of biofeedback. Lilian lived and worked in the Washington, DC area for 60 years until a recent move to the Boston area. A faculty member at Georgetown University Medical School since 1970, she is a Clinical Associate Professor in the Department of Psychiatry.
More personally, Lilian has been on a 22-year glaucoma journey. As she explains it, she wore glasses for reading since age 11, and saw an ophthalmologist annually. But until she suffered an angle closure attack in 1998, she had not been diagnosed with narrow angles.
A narrow angle, which can be detected during a comprehensive eye exam, refers to an angle between the outer edge of the iris and the cornea that is narrower, or more closed, than normal. If not watched, narrow angles can lead to an acute angle attack, which is a medical emergency that can cause permanent damage within hours.
“I am one of those who was only diagnosed after an attack, which partially blinded me,” she says.
Although Lilian lost much vision in her right eye, she praises the glaucoma specialist she began seeing after her attack, who treated her until she moved to Boston in 2016. “That DC doctor is my miracle magician and scientist,” she says.
Lilian has made sure that history does not repeat itself within her family, which includes 4 children and 11 grandchildren, ages 11 to 31. “Given my experience, I easily convinced my family members to be evaluated by a glaucoma specialist. My younger sister and my youngest daughter both have narrow angles. Both had immediate iridotomies and have avoided the potential nightmares of narrow-angle glaucoma.” Lilian’s older grandchildren are proactive as well.
Glaucoma is not the main thread of Lilian’s life. In 2017, she was the recipient of a Lifetime Achievement Award from the Mid-Atlantic Biofeedback Society.
The award was presented “in appreciation and recognition of her contributions to the field of biofeedback, specifically the establishment of one of the country’s first biofeedback programs at Georgetown University Medical School…” according to the certificate.
A related tribute points out that when she set up her first biofeedback clinical program as an elective for medical students in the early 1970’s, biofeedback was still “bio-WHAT?”
Meet Ryan

Twenty-six year old Ryan, who was born with open-angle glaucoma, is well on his way to become an ophthalmologist and give back to the visually impaired community.
A second year medical student at the Medical University of South Carolina, Ryan credits his parents and a great doctor who was able to stabilize his condition very early. In fact, it was the doctor who treated Ryan throughout his childhood and teen years who inspired him to become a physician. “Now I want to help people who weren’t as lucky as I am,” he says.
In Ryan’s case, his parents realized there was something wrong with his eyes shortly after his birth as he was sensitive to light, his eyes were runny, he didn’t want to be outside and looked away from people. They researched the possibilities and suspected he may have glaucoma, which the doctor confirmed. When Ryan was a toddler he had a goniotomy – a surgical procedure used in congenital glaucoma to relieve eye pressure. “Today my pressure is stable, and despite poor vision, I’ve had no major problems. I need glasses to function and I always wear sunglasses when I go outside. The pressure spikes that occurred when I was a baby damaged my vision, but luckily nothing else.”
When Ryan graduated from Clemson University with a degree in bioengineering, he worked in medical device design and development, specifically on neuro (brain and nervous system) devices. He also began volunteering at local eye clinics – helping visually impaired and blind people with tasks and errands. “I saw what they have to go through – and realized how fortunate I am.”
“I also started a program of my own called the Young Eyes Project, where I collect new and used glasses in local schools in Charleston, and then work with a physician at MUSC to give those glasses to children who couldn’t otherwise afford them.”
Appropriately for his desired profession, Ryan will graduate med school in 2020 and then will begin residency work. “I’ll always be involved in research – it’s the most important part of medicine…that’s where everything starts. I also want to be the kind of doctor who is personable. People want a connection and they want to be able to trust that their doctor is doing the right thing for them.”
“When I start practicing, I’ll draw on my own experience to help others with vision problems, having been in their shoes.”
Ryan is currently working on a research project involving medical shunts to relieve pressure in the brain, which can arise from an abnormal buildup of cerebrospinal fluid. The buildup is often caused by an obstruction which prevents proper fluid drainage.
“I think every day about applying this technology to relieve eye pressure in glaucoma. This is life-changing stuff, even when it might not sound exciting. There are lots of possibilities and it’s really frustrating that there is important research going unfunded.”
“The chance that I might lose my vision is always in the back of my mind. But I think I’ll be fine. What I want is to now focus on is helping other people.”
Meet Doug

Doug has been “down the rabbit hole” – and back. He said, “It all started in 2008 when I noticed areas of my vision just weren’t there.”
He saw an eye doctor who gave him a visual field test. Doug said, “I didn’t see the flashing lights, so I thought the machine hadn’t been turned on” and he asked the assistant to retest him. That’s when he realized something was very wrong.
He said, “The doctor showed me the results. I’d lost 90 percent of the vision in my right eye and half in my left. He asked me when I’d last been tested and I said it had been seven or eight years.”
Doug continued, “Heck, I didn’t even know what glaucoma was. There had been no pain or physical sensation to warn me. But my pressures were at 50 and had likely been there for years. The doctor referred me to a glaucoma specialist who said, “I doubt we can save your right eye, but hopefully we can keep the left.”
Doug said, “I was devastated. I think visually and have led a visual life as an outdoor adventurer, photographer, writer and web designer.” As Doug explains in his book From Grief to Grace, “I went down the rabbit hole and into a deep multi-year depression. I lost my home and investments, felt the hand of death reach out to me – and reached back for it.”
But life had other plans. A voice inside him said “do your bucket list,” and it was the pursuit of these adventures that saved his life. The first was kayaking down the Grand Canyon.
It was in a cavern deep within the canyon that he went through what he describes as “the eye of the needle” and found the capacity to transcend the trauma. Second on his bucket list was a two-month adventure odyssey riding a motorcycle on remote dirt roads up the Continental Divide from Mexico to Canada, and using an ancient energy system for personal growth along the way.
His third – and final – bucket list item is to ride a motorcycle from the top of Alaska to the bottom of South America. Doug’s intention is use this adventure as a way to raise awareness about vision issues and trauma-related depression.
And that’s key to Doug’s life today – finding purpose in his life to transcend depression, speaking with others about vision loss and trauma, and inspiring others with stories of hope. He speaks at Lions Clubs in California, co-moderates an online glaucoma support community, and speaks about trauma and depression for counties in Northern California.
One of his key messages is “We can find our greatest gifts in our darkest moments. When you finally get through the darkness, you may find a place of eternal stillness within.”
Thanks to his doctor of many years, he still has some vision in both eyes. He uses three different eye drop medications three times a day. He’s also had a laser treatment, cataract surgery and a trabeculectomy done on his right eye.
What does he suggest for others facing loss of vision? “Reach out, join a group, find support, take care of yourself, and become your own best advocate. And find the best doctor you can.”
Also, you may likely go through the five stages of grief. In my experience, the sooner you begin, the sooner you can get to the other side, find purpose in your life, rise to something higher and be there for others.”
Meet Dave

Fifteen years ago, during an annual eye exam at his optician in England, long-haul truck driver Dave was diagnosed with glaucoma. Only 30 years old, he had been tested routinely as his mother and an aunt had the disease. He was rushed to the hospital for immediate treatment and began taking one, later two and eventually four different medications before trabeculectomy surgery became necessary in both eyes.
“I drive trucks for a living, and have driven on night shifts for 13 of the years since my diagnosis, which probably hasn’t helped my condition,” says Dave. “A few times when I’ve driven long distances at night I found street lights getting misty around them, like a fog, which is when I knew I had a condition that was getting worse.”
Then, in the fall of 2015, just six weeks after a trabeculectomy on his left eye, the doctor said they couldn’t wait the recommended two years before performing the surgery on his right eye.
“I was off work for five months and the government body that controls driving licenses in the UK temporarily revoked my commercial license and my car license as well, pending eye tests, doctors’ reports, medical records, visual field tests. I was left in limbo for months. Work wasn’t paying me so I couldn’t pay my bills and they refused to offer me anything else until we knew whether I would be able to get my license back.
“Even when I successfully reapplied for my license, I had to be assessed by an occupational health expert before work allowed me to drive a truck again. As a result, I no longer work nights, and I work less hours a week than before.
“Living with glaucoma is frustrating, inconvenient, life changing and unpredictable. When my truck driving license is due for renewal in three years, my vision may not be good enough to continue in my chosen profession and I have no other skills.
“I know I have a degenerative and unstable condition that may send me blind. And I don’t want to get to the point where people who know me say things like, ‘Aw, poor Dave, he used to be so active, he used to love flying…driving…martial arts and look at him now, he can’t even cross the road without help!’
“Glaucoma research is extremely important,” he says. “Eyesight is the one sense I couldn’t be without.”
Dave does what he can to preserve his sight, carefully following his medication regimen and changes in his work load. His hope is that increased funding for research will lead to new treatments and a cure soon, as he worries that his son may also develop the disease.
Meet Sherry

Members of online glaucoma support groups may recognize the name of Sherry, a glaucoma patient herself and a patient advocate who is co-owner of one of the major support groups and a member of several others, including The Glaucoma Foundation’s APUP (Adult Patients Under Pressure). Sherry was also a founding board member of the World Glaucoma Patient Association.
A resident of Redmond, Washington, she was diagnosed with glaucoma in 1995. Despite normal pressures while on drops, the doctors noticed progression of damage and she had trabeculectomy surgeries in 2000 and 2001. Since then she’s been doing well. Last fall Sherry had cataract surgery. When you have had trabs, she explains, every surgery on the eye can cause greater risk to the filtering blebs so you need super close follow-up. Sherry didn’t have any complications – the surgery and post-op surgery went smoothly.
It was when Sherry first learned she would have trabeculectomy surgery that she began researching glaucoma and first located a support group. As she says, “I like to learn everything I can about my health issues.” Now she is committed to seeing that other patients are better educated about their glaucoma as well. “Most are afraid to ask questions, and their doctors often don’t take the time to sufficiently communicate with them about the disease. We see it in the support group. Newly diagnosed patients are afraid they will go blind, even though with ongoing treatment less than 10 percent of glaucoma patients lose their sight. They don’t understand the complex and chronic nature of glaucoma and the importance of compliance.”
What would Sherry like to see for better communications between doctors and patients? For a start:
- Patients should talk to their glaucoma specialist and doctors need to be aware of what information patients need.
- Patients should be taught the correct way to use eye drops. (See following article)
- Patients should understand what type of glaucoma they have, possible side effects of their medications, what pressures should be expected, and the prognosis.
- Patients should ask to see test results, for example of their visual fields – with an explanation of what those black spots mean.
- When surgery is scheduled, there should be a conversation beforehand about post-op instructions and what drops they will have to take when.
And here’s some final advice from Sherry: “Understanding that a diagnosis of glaucoma can be scary and stressful and since it’s suspected that IOP can be increased by stress which could intensify progression of damage, it would be good to learn some stress relief techniques to help you relax through this. Some ideas are prayer or meditation, yoga, Tai-Chi or other exercise, massage, a funny movie… And it’s not admitting weakness to even get some counseling from someone who understands low-vision or blindness. I’m sure there are even counselors who have gone through the same thing. Look for a local low-vision group such as The Lighthouse for support. And realize that vision loss does not mean the loss of a productive life but may mean that you need to change how you live!”
Meet David

“A Thirst for Life…”
David of Nashville, Tennessee, age 37, was diagnosed with elevated IOP at the age of 13 and has been on a varying regimen of eye drops ever since.
When he was 27, he had the first of six major eye glaucoma surgeries. This past February, the cornea in his left eye failed. They first needed to move the shunt in that eye to the back of his eye. Then, in May they removed his cornea and iris and implanted a donated cornea.
“Losing my cornea was a real scare. I have a thirst for life. Getting a new cornea renewed that thirst,” says David, who thanks the doctors, nurses, and staff at Vanderbilt University Eye Clinic.
“I try to focus on what I have and remind myself I’m healthy in other ways. I try to be prepared for what would happen if I go completely blind. And I try to stay on top of the latest information.”
David works in sales for an IT company and spends his days in front of a computer screen working from home. “I have limits on how long I can work without a break. But I find ways to cope. I use large fonts on my computer. Technology can help people like me. Things are progressing so quickly.”
Corrected, his vision is 20/40 to 20/60. He’s beginning to lose his peripheral vision but can still drive, even short distances at night. He’s hoping self-driving cars aren’t far off!
“I don’t know how much of my vision will return after this last surgery — it will take about a year to find out. My doctor says I should prepare for the possibility of going blind by my 50s or 60s. But she’s basing that on today’s technology and what we know about the disease right now. I hope things will change. Never say never, right?
“There are so many diseases out there that need funding for research. But glaucoma is an important one. We need more research not less! Glaucoma is constantly on my mind.
“Glaucoma absolutely affects the quality of your life. No, it’s not life-threatening, but it is life-altering. It’s a constant battle. My goal is to maintain what I have.”
Share Your Story
Submit your own story to The Glaucoma Foundation and email cfowkes@glaucomafoundation.org.

